| Structure | Name/CAS No. | Articles |
|---|---|---|
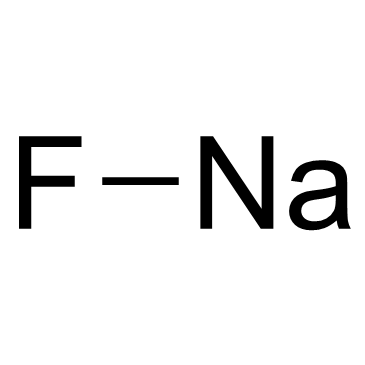 |
Sodium Fluoride
CAS:7681-49-4 |
|
 |
Salbutamol
CAS:18559-94-9 |
|
 |
Water
CAS:7732-18-5 |
|
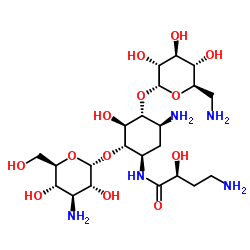 |
Amikacin
CAS:37517-28-5 |
|
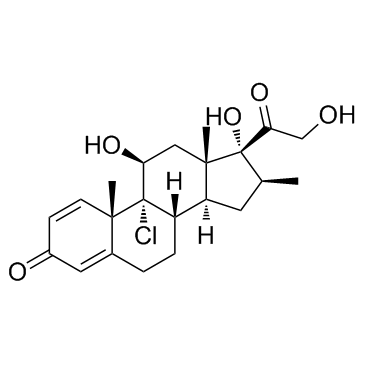 |
Beclometasone
CAS:4419-39-0 |